Crowson, M. G. et al. A contemporary review of machine learning in otolaryngology–head and neck surgery. Laryngoscope 130, 45–51 (2020).
Bur, A. M., Shew, M. & New, J. Artificial intelligence for the otolaryngologist: a state of the art review. Otolaryngol. Neck Surg. 160, 603–611 (2019).
Liu, G. S., Jovanovic, N., Sung, C. K. & Doyle, P. C. A scoping review of artificial intelligence detection of voice pathology: challenges and opportunities. Otolaryngol. Neck Surg. 171, 658–666 (2024).
Artificial Intelligence and Machine Learning (AI/ML)-Enabled Medical Devices. FDA https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-aiml-enabled-medical-devices (2024).
ENT Navigation Application with Kick EM from Brainlab. Brainlab https://www.brainlab.com/surgery-products/overview-ent-products/ent-navigation-application/.
Reimagining the Way Medical Devices Are Designed. PacificMD Biotech https://www.pmdbiotech.com/.
Lu, J. H. et al. Assessment of adherence to reporting guidelines by commonly used clinical prediction models from a single vendor: a systematic review. JAMA Netw. Open 5, e2227779 (2022).
Vasey, B. et al. Reporting guideline for the early-stage clinical evaluation of decision support systems driven by artificial intelligence: DECIDE-AI. Nat. Med. 28, 924–933 (2022).
Gajecki, T., Zhang, Y. & Nogueira, W. A deep denoising sound coding strategy for cochlear implants. IEEE Trans. Biomed. Eng. 70, 2700–2709 (2023).
Raghavan, A. M., Lipschitz, N., Breen, J. T., Samy, R. N. & Kohlberg, G. D. Visual speech recognition: improving speech perception in noise through artificial intelligence. Otolaryngol. -Head. Neck Surg. J. Am. Acad. Otolaryngol. -Head. Neck Surg. 163, 771–777 (2020).
Healy, E. W., Taherian, H., Johnson, E. M. & Wang, D. A causal and talker-independent speaker separation/dereverberation deep learning algorithm: Cost associated with conversion to real-time capable operation. J. Acoust. Soc. Am. 150, 3976 (2021).
Cohen, J. F. et al. STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open 6, e012799 (2016).
Collins, G. S., Reitsma, J. B., Altman, D. G. & Moons, K. G. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMC Med. 13, 1 (2015).
Des Jarlais, D. C., Lyles, C. & Crepaz, N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am. J. Public Health 94, 361–366 (2004).
von Elm, E. et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335, 806–808 (2007).
Liu, X., Cruz Rivera, S., Moher, D., Calvert, M. J. & Denniston, A. K. Reporting guidelines for clinical trial reports for interventions involving artificial intelligence: the CONSORT-AI extension. Nat. Med. 26, 1364–1374 (2020).
Liu, Y., Chen, P.-H. C., Krause, J. & Peng, L. How to read articles that use machine learning: users’ guides to the medical literature. JAMA 322, 1806–1816 (2019).
Selvaraju, R. R. et al. Grad-CAM: visual explanations from deep networks via gradient-based localization. Int. J. Comput. Vis. 128, 336–359 (2020).
Zhou, B., Khosla, A., Lapedriza, A., Oliva, A. & Torralba, A. Learning Deep Features for Discriminative Localization. In 2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR) 2921–2929 (IEEE, 2016). https://doi.org/10.1109/CVPR.2016.319.
Kamran, F. et al. Evaluation of sepsis prediction models before onset of treatment. NEJM AI 1, AIoa2300032 (2024).
Ruamviboonsuk, P. et al. Real-time diabetic retinopathy screening by deep learning in a multisite national screening programme: a prospective interventional cohort study. Lancet Digit. Health 4, e235–e244 (2022).
Lind Plesner, L. et al. Commercially available chest radiograph AI tools for detecting airspace disease, pneumothorax, and pleural effusion. Radiology 308, e231236 (2023).
Gomez Rossi, J., Rojas-Perilla, N., Krois, J. & Schwendicke, F. Cost-effectiveness of artificial intelligence as a decision-support system applied to the detection and grading of melanoma, dental caries, and diabetic retinopathy. JAMA Netw. Open 5, e220269 (2022).
Seneviratne, M. G., Shah, N. H. & Chu, L. Bridging the implementation gap of machine learning in healthcare. BMJ Innov. 6, 45–47 (2020).
Mennella, C., Maniscalco, U., De Pietro, G. & Esposito, M. Ethical and regulatory challenges of AI technologies in healthcare: a narrative review. Heliyon 10, e26297 (2024).
Crowson, M. G. & Rameau, A. Standardizing machine learning manuscript reporting in otolaryngology-head & neck surgery. Laryngoscope 132, 1698–1700 (2022).
Callahan, A. et al. Standing on FURM ground: a framework for evaluating fair, useful, and reliable AI models in health care systems. NEJM Catal. Innov. Care Deliv. 5, https://doi.org/10.1056/CAT.24.013 (2024).
Liu, G. S. et al. Deep learning classification of inverted papilloma malignant transformation using 3D convolutional neural networks and magnetic resonance imaging. Int. Forum Allergy Rhinol. 12, 1025–1033 (2022).
Liu, G. S. et al. ELHnet: a convolutional neural network for classifying cochlear endolymphatic hydrops imaged with optical coherence tomography. Biomed. Opt. Express 8, 4579–4594 (2017).
Liu, G. S., Shenson, J. A., Farrell, J. E. & Blevins, N. H. Signal to noise ratio quantifies the contribution of spectral channels to classification of human head and neck tissues ex vivo using deep learning and multispectral imaging. J. Biomed. Opt. 28, 016004 (2023).
Shenson, J. A., Liu, G. S., Farrell, J. & Blevins, N. H. Multispectral imaging for automated tissue identification of normal human surgical specimens. Otolaryngol. Head. Neck Surg. J. Am. Acad. Otolaryngol. Head. Neck Surg. 164, 328–335 (2021).
Liu, G. S. et al. End-to-end deep learning classification of vocal pathology using stacked vowels. Laryngoscope Investig. Otolaryngol. 8, 1312–1318 (2023).
Liu, G. S., Cooperman, S. P., Neves, C. A. & Blevins, N. H. Estimation of cochlear implant insertion depth using 2D-3D registration of postoperative X-ray and preoperative CT images. Otol. Neurotol. 45, e156 (2024).
Neves, C. A. et al. Automated radiomic analysis of vestibular Schwannomas and inner ears using contrast-enhanced T1-weighted and T2-weighted magnetic resonance imaging sequences and artificial intelligence. Otol. Neurotol. 44, e602 (2023).
Liu, G. S. et al. Artificial intelligence tracking of otologic instruments in mastoidectomy videos. Otol. Neurotol. 45, 1192 (2024).
Youssef, A. et al. External validation of AI models in health should be replaced with recurring local validation. Nat. Med. 29, 2686–2687 (2023).
Granlund, T., Stirbu, V. & Mikkonen, T. Towards regulatory-compliant MLOps: Oravizio’s journey from a machine learning experiment to a deployed certified medical product. SN Comput. Sci. 2, 342 (2021).
Beswick, D. M. et al. Design and rationale of a prospective, multi-institutional registry for patients with sinonasal malignancy. Laryngoscope 126, 1977–1980 (2016).
Crowson, M. G. et al. A systematic review of federated learning applications for biomedical data. PLOS Digit. Health 1, e0000033 (2022).
Warnat-Herresthal, S. et al. Swarm Learning for decentralized and confidential clinical machine learning. Nature 594, 265–270 (2021).
Holm, E. A. In defense of the black box. Science 364, 26–27 (2019).
Ghassemi, M., Oakden-Rayner, L. & Beam, A. L. The false hope of current approaches to explainable artificial intelligence in health care. Lancet Digit. Health 3, e745–e750 (2021).
Ayoub, N. F., Lee, Y.-J., Grimm, D. & Balakrishnan, K. Comparison between ChatGPT and Google search as sources of postoperative patient instructions. JAMA Otolaryngol. Neck Surg. 149, 556–558 (2023).
Vaira, L. A. et al. Validation of the quality analysis of medical artificial intelligence (QAMAI) tool: a new tool to assess the quality of health information provided by AI platforms. Eur. Arch. Otorhinolaryngol. 281, 6123–6131 (2024).
Vaira, L. A. et al. Enhancing AI Chatbot responses in health care: the SMART prompt structure in head and neck surgery. OTO Open 9, e70075 (2025).
Judge, C. S. et al. Multimodal artificial intelligence in medicine. Kidney360 5, 1771 (2024).
Frosolini, A. et al. Artificial intelligence in audiology: a scoping review of current applications and future directions. Sensors 24, 7126 (2024).
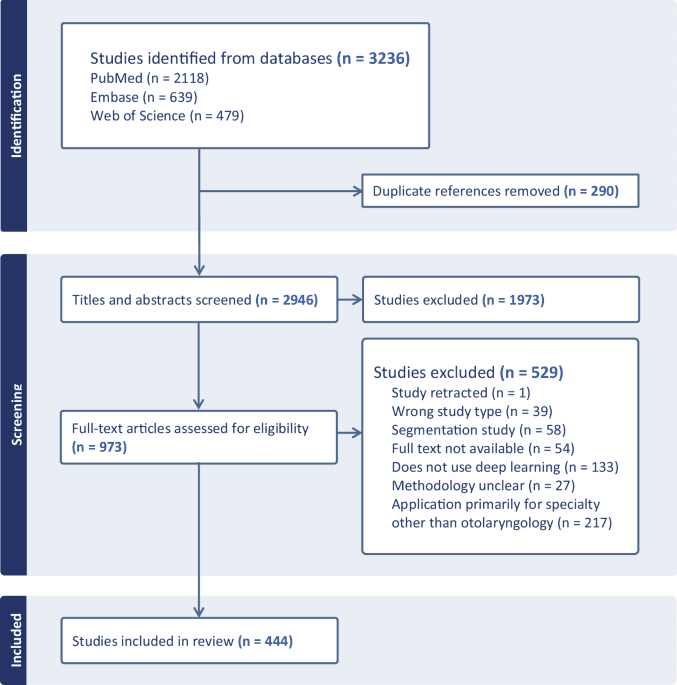
Tricco, A. C. et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 169, 467–473 (2018).
Covidence systematic review software. Veritas Health Innovation.