This section presents the results of a study that examined how AI-powered assistive tools affected the mobility and daily tasks of children with Down syndrome in Saudi Arabia. The study used both quantitative survey data (n = 123) and qualitative insights from seven interviews with the caregivers.
Quantitative results
Table 2 provides an overview of the demographic characteristics of the participants, offering insights into the distribution of AI-assistive tool users compared to non-users. In terms of gender distribution, the proportions were relatively balanced, with males representing 60% of AI users and 58% of non-users. This suggests that gender does not play a significant role in the adoption of AI-assistive tools.
Regarding the age distribution of children with Down syndrome, the majority fall within the 5–10 years category (36% of AI users and 37% of non-users), followed by the 11–15 years category (32% and 24%, respectively). This indicates that AI adoption is widespread across age groups. However, a slightly higher percentage of younger children (under five years) was found among non-users (25%), which suggests that families with younger children are more hesitant to integrate AI tools at an early stage.
Table 2 also reveals notable differences in educational levels between the two groups. AI users tended to have higher educational qualifications, with 38% holding a bachelor’s degree and 28% possessing postgraduate qualifications. In contrast, non-users were more concentrated in lower education levels, particularly at the diploma (30%) and high school (22%) levels. This pattern suggests that higher education may be associated with greater awareness of and willingness to adopt AI-powered assistive tools.
Economic status also appears to influence AI adoption. A significant proportion of AI users fell within the income bracket of 10,001–15,000 SAR (40%), with 32% earning more than 15,000 SAR. In contrast, 43% of non-users belong to the lower-income bracket of 5,000–10,000 SAR. This difference indicates that financial constraints may be a limiting factor in AI adoption because families with higher income levels may have greater access to these technologies.
Table 2 shows that there are only small differences in where AI users and non-users live. Most of the participants live in Riyadh (66% of AI users and 63% of non-users), while the rest are from Al-Jouf. This means that cities like Riyadh may have easier access to AI tools that can help people than less developed areas. This could change the number of places that use these technologies and how widely they are used.
Participant characteristics
This study recruited 123 parents and carers of children diagnosed with Down syndrome, comprising 47 families actively using AI-powered assistive tools and 76 families not using such technologies. While participants were not randomly assigned to groups (as AI usage was self-selected), we ensured group comparability by matching on key child characteristics, including age, cognitive functioning level, physical mobility status, and associated medical conditions. Demographic differences between groups (parental education and income) were treated as covariates in subsequent analyses to control for potential confounding effects.
The baseline characteristics of the participating children were assessed to ensure group comparability (Table 3). Cognitive functioning levels were distributed similarly across both groups, with approximately half of the participants in each group classified as having moderate intellectual disability (IQ 35–49). Mild intellectual disability (IQ 50–70) was observed in 32% of AI users compared to 29% of non-users, while severe intellectual disability (IQ 20–34) affected 17% and 21%, respectively. Chi-square analysis revealed no significant difference in the cognitive functioning distribution between the groups (χ² = 0.625, p = 0.732).
Physical mobility status also demonstrated comparable distributions between the groups. Independent walking was achieved by 60% of the children in the AI user group and 57% in the non-user group. Approximately one-third of the participants in both groups required assisted walking with support (32% AI users, 34% non-users), while non-ambulatory status requiring wheelchair dependence was observed in 8% and 9% of participants, respectively. Statistical analysis confirmed no significant differences in the mobility status (χ² = 0.937, p = 0.627).
The associated medical conditions commonly observed in Down syndrome were similarly distributed between the groups. Congenital heart disease affected approximately one-quarter of the participants in both groups (26% AI users and 25% non-users, p = 0.925). Hearing impairments were present in 17% and 18% of AI users and non-users, respectively (p = 0.856), while vision problems affected 13% and 14% of AI users and non-users, respectively (p = 0.813). Hypothyroidism was diagnosed in 23% of AI users compared to 26% of non-users (p = 0.714). No medical conditions showed statistically significant differences between the groups.
Communication abilities were assessed across three categories, with verbal communication being the most common ability in both groups (62% of AI users, 58% of non-users). Limited verbal communication with gesture support was observed in 30% of AI users and 34% of non-users, whereas nonverbal communication affected 8% of participants in both groups. Chi-square analysis revealed no significant differences in communication ability (χ² = 1.125, p = 0.569).
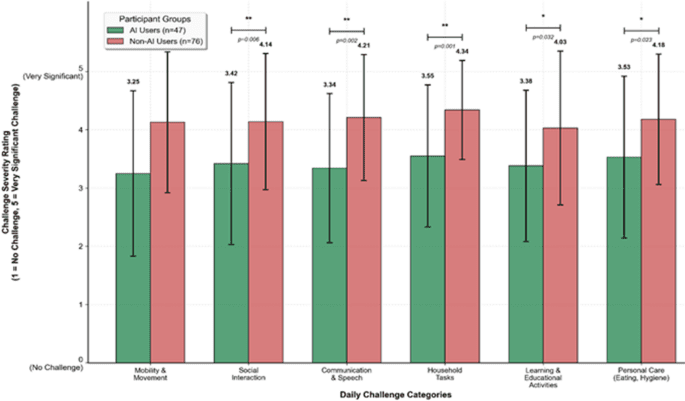
A 5-point Likert scale was used to compare daily challenges faced by children with Down syndrome between AI users and non-users. The results are presented in Table 4. The results show that people who do not use AI face many more problems in every area. The largest differences were observed when doing household tasks (M = 4.34, SD = 0.85, p = 0.001), talking and communicating (M = 4.21, SD = 1.08, p = 0.002), and moving around (M = 4.13, SD = 1.21, p = 0.004). These statistically significant differences are consistent with the hypothesis that AI-powered assistive technologies may help mitigate challenges in these areas, though causality cannot be established based on cross-sectional data.
Among AI users, the reported difficulty levels were lower, with mean scores ranging from 3.25 to 3.55, indicating moderate challenges rather than severe ones. The lowest reported challenge among AI users was mobility and movement (M = 3.25, SD = 1.42), suggesting that walk-assist devices may have a positive impact on enhancing mobility and coordination. Additionally, AI users reported lower challenges in communication (M = 3.34, SD = 1.28), which are likely to reflect the benefits of AI-powered communication apps in improving speech and interaction.
Statistical analysis supported these observations. The T-test results (p < 0.05) showed that AI users and non-users were significantly different in all categories. Levene’s test results confirmed that the variances between the two groups were comparable, thus ensuring the reliability of the findings. Cohen’s d effect sizes range from 0.49 to 0.83, which indicates moderate to large effects. The most noticeable effect was observed when AI was used to do housework (d = 0.83), which supports AI’s role in encouraging independence.
Despite these benefits, both groups continued to report moderate challenges in personal care (M = 3.53 for AI users, M = 4.18 for non-users) and learning activities (M = 3.38 for AI users, M = 4.03 for non-users). This means that AI-based assistive technologies may help in some ways but may not completely address challenges in self-care and educational activities.
Comparison of Daily Challenge Severity Between AI Users and Non-AI Users. Comparative analysis of daily challenge severity ratings across six functional domains between AI technology users (n = 47) and non-users (n = 76). Challenge severity was measured on a 5-point Likert scale (1 = No Challenge, 5 = Very Significant Challenge). Error bars represent standard deviations. Asterisks indicate statistical significance levels: *p < 0.05, **p < 0.01. AI users consistently reported lower challenge severity across all domains, with statistically significant differences observed in all categories (p < 0.05).
Figure 1 demonstrates a consistent and statistically significant pattern wherein AI technology users report substantially lower daily challenge severity across all measured domains than non-users. The magnitude of the difference was particularly pronounced in household tasks (AI users: M = 3.55, non-AI users: M = 4.34, p < 0.001) and communication challenges (AI users: M = 3.34, non-AI users: M = 4.21, p < 0.01). These findings suggest that AI-assistive technologies may provide meaningful functional benefits in reducing perceived challenge severity across multiple life domains. The consistency of this pattern across diverse functional areas, from mobility and social interaction to personal care, indicates that AI technology adoption may have a broad positive impact on daily functioning in children with Down syndrome.
Figure 2 shows AI-powered assistive tool distribution among participants, with smart communication apps most commonly used (36%), followed by AI-powered learning apps (26%) and smart home assistants (17%). These patterns suggest carers prioritise tools enhancing communication, education, and daily task management, aligning with reported challenges. Lower adoption rates for walk-assist devices (9%) and social-assistive robots (6%) may reflect cost barriers, limited accessibility, or effectiveness uncertainty. Despite mobility being a major challenge among non-AI users, low walk-assist device adoption suggests access or awareness limitations. Similarly, social assistive robots remain underutilised despite their interaction benefits, possibly due to high costs or limited availability in the study area. The custom tools category (6%) indicates some families use specialised solutions tailored to individual needs, highlighting assistive technology adoption’s individualised nature, where standard solutions may not meet each child’s unique requirements.
Distribution of AI-powered assistive technology Categories Among Study Participants. Frequency distribution of AI assistive tools used by families with Down syndrome children (n = 47). Bars show number of users and percentage for each technology category, ranked by adoption rate. Smart communication apps were most commonly used (17 users, 36%), while social assistive robots and custom solutions had the lowest adoption (3 users each, 6%). Representative examples of tools within each category are shown in parentheses.
Table 5 demonstrates patterns in AI-powered assistive technology adoption sustainability, with usage duration following a declining trajectory, where only 13% of participants maintained usage beyond 24 months compared to 38% in the 6–12 month range, indicating significant long-term retention challenges. Implementation occurs predominantly in home environments (89%), with tool-specific variations reflecting functional characteristics. Walk-assist devices show the highest clinical involvement (25%) because of their medical nature, while smart home assistants and social assistive robots demonstrate exclusive domestic usage (100%), and communication apps remain largely home-centred (94%). The statistically significant relationship between usage duration and perceived effectiveness (F(3,43) = 4.567, p = 0.008, η² = 0.242) suggests that sustained engagement enhances outcomes, with an effectiveness variance attributable to usage duration of approximately 24%.
Table 6 presents the perceived effectiveness of AI-assistive tools across four key areas: mobility, daily independence, social interaction, and overall quality of life. The ratings, based on a 5-point Likert scale, indicate moderate to high effectiveness, with mean scores ranging between 3.68 and 3.85.
The category with the most votes (M = 3.85, SD = 0.93) was “increasing daily independence.” This means that AI tools, especially smart home assistants and AI-powered learning apps, are seen as helpful in helping children perform daily tasks with less help from carers. The relatively low standard deviation (0.93) indicated greater agreement among participants regarding the effectiveness of these tools.
Improving mobility (M = 3.78, SD = 1.18) also received a relatively high score, reflecting the positive impact of walk-assist devices for children with Down syndrome. A higher standard deviation (1.18) suggests that the responses varied more. This could be because people have different mobility needs or difficulties accessing these devices.
Enhancing social interaction (M = 3.68, SD = 1.40) had the lowest mean score, indicating that, while smart communication apps and social assistive robots provide some benefits, their effectiveness may vary depending on the child’s individual needs and the tool’s usability. The higher standard deviation (1.40), which also suggests that user experiences are different, could be due to factors such as how responsive the child is to AI-driven social interactions or how difficult it is for them to use these tools effectively.
Improving the overall quality of life (M = 3.80, SD = 1.17) received a slightly higher rating, reflecting the general positive impact of AI-assistive tools across multiple domains. Moderate standard deviation indicates some variability in perceived benefits, which may be influenced by the extent of tool adoption and integration into daily routines.
Table 7 highlights the key challenges in using AI assistive tools, with high cost (74.46%) being the most significant barrier, limiting accessibility for many families. Lack of technical support (38.29%) and difficulty adapting to technology (31.91%) indicated that usability and training remain concerns. Additionally, software issues (25.53%) and device incompatibility (21.27%) suggested that not all AI tools meet individual needs. These findings emphasise the need for financial assistance, better user support, and improved customisation to enhance the effectiveness and accessibility of AI-assistive tools.
Figure 3 presents a comparative analysis of adoption barriers and corresponding solution preferences among families currently not using AI-assisted technologies. Visualisation reveals important insights into intervention opportunities by juxtaposing barrier prevalence with solution appeal across the five key domains.
Infrastructure and access limitations demonstrated the highest intervention potential, with a net impact on + 16 families (+ 21.1%). While only 22 families (28.9%) cited this as a barrier, 38 families (50.0%) expressed an interest in education and skill development programs, suggesting that targeted training initiatives could address broader adoption challenges beyond immediate infrastructure concerns.
Financial constraints, though affecting the largest proportion of families (38 families, 50.0%), show more modest intervention potential (+ 7 families, + 9.2%) due to the correspondingly high interest in financial support programs (45 families, 59.2%). This indicates that, while financial barriers are widespread, the proposed solutions align well with the identified needs.
Technology dependency fears presented a concerning pattern, being the only category with a negative net impact (-5 families, -6.5%). The limited appeal of custom incentives (10 families, 13.2%) relative to the prevalence of technology fears (15 families, 19.7%) suggests that this barrier may require more innovative intervention approaches that are not captured in conventional solution categories.
Awareness and trust issues and scepticism concerns both demonstrated positive but moderate intervention potential (+ 7 and + 10 families, respectively), indicating that trial-based programs and community validation strategies could effectively address these barriers.
Qualitative results
To gain more profound insights into the experiences of parents using AI-powered assistive tools for their children with Down syndrome, semi-structured interviews were conducted with seven carers (see Table 8). The interviews aimed to explore the perceived benefits, challenges, and factors influencing the adoption and continued use of AI-based assistive technologies. The data were analysed using thematic analysis, which allowed the identification of key themes emerging from the participant responses. The qualitative findings provide additional perspectives that were not fully captured in the quantitative survey, particularly regarding the emotional and psychological impacts of AI tools on carers and their children.
Perceived benefits of AI assistive tools
Participants generally expressed satisfaction with the impact of the AI-powered assistive tools on their children’s daily activities, communication, and independence. Many parents noted that these technologies provided tangible improvements in mobility, learning, and social interaction, ultimately enhancing their children’s ability to navigate their daily lives more effectively. The most frequently reported benefit was enhanced mobility, particularly among parents whose children use walk-assist devices. These tools not only helped children improve their physical movement but also contributed to greater confidence and willingness to explore their surroundings. One participant highlighted the transformation.
“Since using the robotic walking aid, my child has become more eager to move independently, which was not the case before.” (P2).
In addition to mobility improvements, smart communication apps have been widely valued, especially by parents of nonverbal children. These technologies allow children to express their needs, emotions, and preferences more clearly, reducing frustration for both the child and the carer. Improved communication has a direct impact on family interactions, fostering meaningful engagement between the child and their surroundings. A carer shared:
“Before using the communication app, my child struggled to communicate his needs. Now, he points at the screen, and we understand him much faster.” (P1).
Beyond the direct benefits for children, the qualitative findings also revealed an important new insight that was not captured in the quantitative data: the emotional relief experienced by carers. Several parents have reported that AI tools contribute to a noticeable reduction in caregiving stress. As these technologies enable their children to engage in self-care activities and structured learning independently, parents experience less pressure and mental exhaustion associated with constant supervision. This shift allowed carers to allocate more time to other responsibilities while feeling reassured of their children’s engagement. One mother described this change as follows:
“With the AI learning app, my child stays engaged and enjoys the lessons, giving me time to focus on other tasks.” (P3).
This suggests that the impact of AI tools extends beyond the child, influencing the broader family dynamics and the overall well-being of carers. By reducing the daily burden of caregiving, these technologies create a more balanced environment for both parents and children, demonstrating the secondary but equally important benefit of AI-powered assistive tools.
Challenges in using AI assistive tools
Despite the numerous benefits reported by parents, the adoption and integration of AI-powered assistive tools into daily routines present several challenges. One of the most frequently cited barriers is cost, which limits access to AI tools for many families. The financial burden associated with purchasing and maintaining these technologies was described as a significant obstacle, preventing some families from adopting them or restricting the range of tools that they could afford. One participant explained,
“We had to make financial sacrifices to afford these tools, and not all families can do that.” (P5).
Beyond affordability, technical difficulties have emerged as major concerns. Many parents struggle with frequent software updates, troubleshooting errors, and a lack of adequate customer support, making it difficult to use AI tools effectively. Some reported frustration with the absence of clear guidance or assistance, which made it challenging to resolve technical issues independently. One participant shared their experiences with a smart home assistant, stating:
“When the smart home assistant stopped responding, I had no idea how to fix it, and there was no clear guidance available.” (P4).
This indicates that while AI assistive tools have the potential to significantly improve children’s independence and quality of life, their effectiveness is often contingent on the level of technical support available to carers.
Another major challenge was child adaptation and engagement, which varied significantly across the families. While some children quickly embraced AI tools, others showed resistance or required extended adjustment periods before they could comfortably use the technology. Parents noted that some children, particularly those with sensory sensitivities or aversion to change, initially rejected AI devices and required gradual exposure and encouragement. One participant described their child’s reluctance to use a mobility-assistive device:
“At first, my child refused to wear the mobility device, and it took weeks of encouragement before he started using it comfortably.” (P2).
This finding suggests that the successful integration of AI tools may require structured behavioural strategies, such as gradual exposure, positive reinforcement, and tailored support from therapists or educators. Given that each child responds differently to technology, a one-size-fits-all approach may not be effective, thus emphasizing the need for customizable solutions and adaptive training programs to facilitate a smoother transition.
Overall, the challenges identified by parents highlighted three key areas for improvement: financial accessibility, enhanced technical support, and structured adaptation strategies. Addressing these barriers could significantly improve the long-term effectiveness and usability of AI-powered assistive tools, making them more accessible and beneficial to children with Down syndrome and their families.
Factors influencing adoption and continued use
Several key factors were identified as critical motivators for the adoption and continued use of AI-powered assistive tools. Government financial support was highlighted as a primary enabler, with one parent stating:
“If financial aid were available, I believe more families would adopt these technologies.” (P6).
Additionally, training programs for parents and carers are essential for effective use. Participants emphasised that many AI tools require technical knowledge that parents may lack, making educational support crucial.
Peer recommendations also play a significant role in shaping the adoption decisions. Many carers reported that they initially hesitated to use AI tools but were persuaded by success stories from other families or professionals. One participant noted:
“I was sceptical at first, but after hearing another parent’s experience, I decided to give it a try, and it has been life-changing.” (P7).
A new finding, not evident in the quantitative analysis, was that some parents experienced a shift in perception regarding technology dependence. Initially, there was a concern that AI tools might create over-reliance, but over time, many parents viewed them as complementary rather than replacing parental interaction. One participant expressed the following:
“At first, I worried that my child would become too dependent on the AI assistant, but now I see it as a helpful tool rather than a replacement for family engagement.” (P4).
This suggests that initial hesitation about AI reliance may diminish over time, as carers experience tangible benefits.
These qualitative findings reinforce the survey results, confirming that AI-powered assistive tools significantly enhance mobility, communication, and independence in children with Down syndrome. However, the interviews provided additional insights that were not captured in quantitative data, particularly in relation to the emotional relief experienced by carers and the evolving perceptions of AI reliance.
Although financial constraints and technical barriers remain substantial obstacles, the qualitative results highlight the importance of structured training programs, peer networks, and government financial support in ensuring successful adoption. Addressing these factors could broaden accessibility and improve the long-term impact of AI-powered assistive technologies on both children and their families.